Revolutionizing Medical Education with XR
By Meryem T. Ok, MD, PhD
Medical education has long relied on trusted tools like textbooks, 2D images, and cadaver labs to teach anatomy, procedures, and foundational knowledge. While these methods remain essential, Extended Reality (XR), encompassing Augmented Reality (AR), Virtual Reality (VR), and Mixed Reality (MR), is revolutionizing medical education by enhancing traditional learning methods through immersive training experiences. This technology not only enriches hands-on learning but also expands access to high-quality education, particularly in settings where resources may be limited.

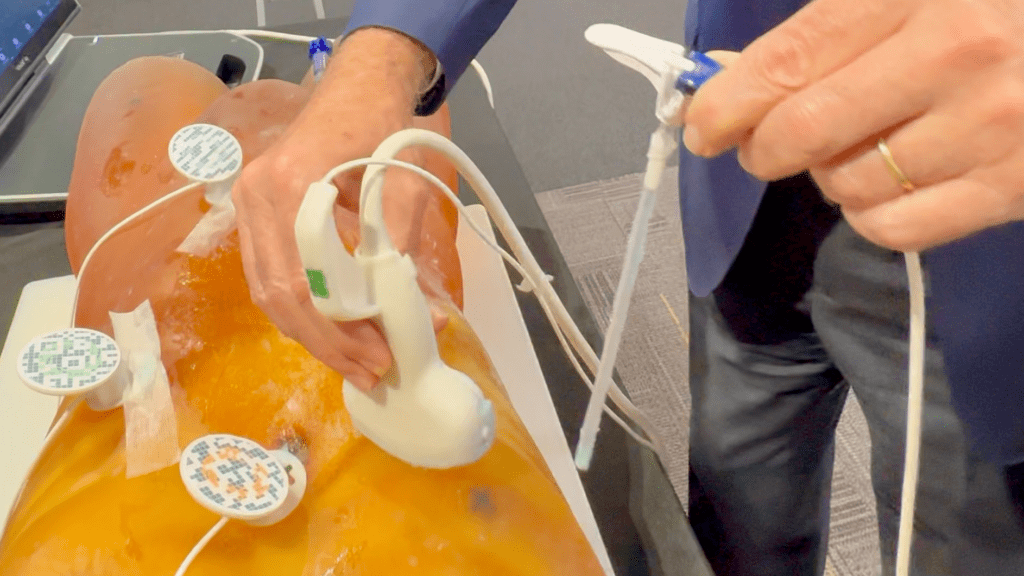
Hololens Utrasound
Ultrasound Training
For example, in ultrasound training, XR technologies provide real-time visual overlays that guide learners in probe placement, image interpretation, and spatial orientation. A recent pilot study demonstrated that AR visualization significantly improved trainee performance and reduced cognitive load during ultrasound-guided interventions, highlighting the effectiveness of AR in enhancing medical education (Liao et al.).
Anatomy Education
In anatomy education, XR complements cadaver labs and static 2D images by offering dynamic, three-dimensional visualizations of human structures. This platform allows students to interact with and explore anatomical details layer by layer, rotate organs, and observe physiological processes like blood flow in health and disease. An integrative review found that XR is commonly reported in anatomical education and may be as effective as traditional teaching methods, underscoring its value as a cost-effective, scalable tool that provides an accessible means of curriculum delivery (Curran et al.).
Procedural Training
Procedural training for techniques like endoscopies and biopsies benefits immensely from XR’s immersive simulations. By creating realistic clinical scenarios with haptic feedback, much like the buzzing in the classic board game “Operation,” XR enables learners to practice navigating internal structures and performing precise interventions in a risk-free, virtual environment. A systematic review of the utility of XR in radiology education and image-guided training suggests that such technologies can significantly enhance surgical and procedural proficiency while preparing trainees for rare or high-risk medical situations (Lang et al.).
VRT-U is committed to leveraging XR to deliver medical training that is immersive, adaptable, and scalable. By complementing traditional educational tools, XR ensures that trainees can gain the skills they need—anywhere, anytime—thereby expanding access to high-quality medical education, especially in resource-limited settings. As these technologies continue to advance, they aim to prepare future healthcare providers more effectively, striving for improved patient outcomes and safer delivery of care.
Sources Cited:
- Liao, S. C., Shao, S. C., Gao, S. Y., et al. “Augmented Reality Visualization for Ultrasound-Guided Interventions: A Pilot Randomized Crossover Trial to Assess Trainee Performance and Cognitive Load.” BMC Medical Education, vol. 24, no. 1, 2024, p. 1058. BioMed Central, https://doi.org/10.1186/s12909-024-05998-8.
- Curran, V. R., Xu, X., Aydin, M. Y., et al. “Use of Extended Reality in Medical Education: An Integrative Review.” Medical Science Educator, vol. 33, no. 1, 2023, pp. 275–286. SpringerLink, https://doi.org/10.1007/s40670-022-01698-4.
- Lang, Min, et al. “Medical Extended Reality for Radiology Education and Training.” Journal of the American College of Radiology, vol. 21, no. 10, 2023, pp. 1583–1594. ScienceDirect, https://doi.org/10.1016/j.jacr.2024.05.006.
